OTTAWA – The Atlas Institute for Veterans and Families and Wounded Warriors Canada today announced the expansion of Introduction to trauma-exposed professionals, an online course developed to increase health care providers’ understanding of the unique cultural differences experienced by trauma-exposed professionals due to the high demand for the training.
In May 2022, supported and funded by the Atlas Institute, Wounded Warriors Canada released Introduction to trauma-exposed professionals, a course developed by Wounded Warriors Canada’s National Clinical Director, Dr. Tim Black to provide culturally specific clinical approaches for supporting this unique population which includes military, Veteran, first responder and police populations. When the first training was released there was immediate national demand, and to date more than 1,600 providers have completed the course.
In response to the demand the Atlas Institute provided additional funding to produce Introduction to trauma-exposed professionals in French which will make the course available in both official languages. Both will continue to be provided at no cost to eligible health care providers for the next two years while the two organizations continue to work together to produce additional modules. The French version of TeXP will be made available at a later date.
Scott Maxwell, Executive Director of Wounded Warriors Canada, commented, “Working with the Atlas Institute is a great example of how partnerships serve as force multipliers for service delivery. We’re thrilled by the response we have received since we launched Introduction to trauma-exposed professionals, which has served to reinforce how much the health care community cares about the mental health supports provided to our injured Veterans, first responders and their Families. We look forward to expanding access to this important training across the country.”
MaryAnn Notarianni, Deputy CEO and Executive Vice-President, Knowledge Mobilization at the Atlas Institute, commented, “We have been so encouraged by the interest from health care providers to access Introduction to trauma-exposed professionals. The feedback on the course has demonstrated its relevance and effectiveness. We want to continue building on this momentum for Veterans of the Canadian Armed Forces and Royal Canadian Mounted Police, first responders and their Families. We’re so pleased to build on our productive partnership with Wounded Warriors Canada to develop a version of this excellent course completely in French and to enable access to any interested and eligible clinicians and health care providers over the next two years for both the English and French versions.”
Ottawa, ON – April 23, 2024 – After leaving the Canadian Armed Forces (CAF), Veterans have reported experiencing challenges in several areas in their lives, from employment to loss of identity. There has been an increase in Canadian research about the transition from military to post-service life in order to understand the factors that promote an optimal transition, but women’s specific experiences remain understudied. For this reason, the Canadian Legacy Project has partnered with the Atlas Institute for Veterans and Families to conduct a study on the experiences of women Veterans during their transition from the military.
Fardous Hosseiny, President and CEO of the Atlas Institute, referred to this as a much-needed initiative, adding, “We know that women Veterans’ experiences can be different from that of men Veterans and that research is needed to inform tailored programming and supports for women who have transitioned — and are in the process of transitioning — to post-military life,” he said. “We expect the partnership with the Canadian Legacy Project will help identify some of the critical factors that impact transition and generate evidence to enhance the design of programs and supports.”
This study, which is being commissioned by the Canadian Legacy Project, will fall under the Atlas Institute’s broader program of research on women Veterans’ health and well-being. Dr. Sara Rodrigues, Director of Applied Research of the Atlas Institute added: “There is much that remains to be done for women Veterans to receive the support and care they need and deserve. Our goal is to work with women Veterans, amplifying their voices to inform research and initiatives and ensure they reflect their needs and priorities.”
“The increase of women enrollment in the Canadian military is reshaping the Veteran population. Women Veterans’ unique experiences can impact healthcare programs and this research will go a long way to ensure that their feedback helps shape the supports require to help them successfully transition back to civilian life.” David Howard, Founder and President of the Canadian Legacy Project noted. “Unfortunately our women Veterans are more likely to experience some types of traumatic events, such as sexual assault, during their service that is associated with a high risk for developing posttraumatic stress disorder (PTSD).” Howard added.
Recruitment is set to begin in the near future and will be communicated through the Atlas Institute’s and the Canadian Legacy Project’s channels once it has started.
For more information, contact: media-atlas@theroyal.ca
Or
David Howard
Founder and President
Canadian Legacy Project
(403) 620-4255
www.canadianlegacy.org
ABOUT THE CANADIAN LEGACY PROJECT
The Canadian Legacy Project is a national registered charity established in 2008 to support Canadian Veterans in their time of need and advocate on their behalf. The Canadian Legacy Project builds, directs and supports free programs for our Canadian Veterans to help them successfully transition back to civilian life. In parallel to this, the Canadian Legacy Project works with Canadas’ youth to educate them about the heroism and sacrifice made by our Canadian Veterans.
Quick Facts:
- The Canadian Legacy Project provides free access to important services for Veterans, including housing, education, training, support services, programing and supports specific to women Veterans.
- The Canadian Legacy Projects’ Business Boot Camp has become the fastest growing and most successful entrepreneurial training program for Canadian Veterans looking to start their own business.
- The Canadian Legacy Project continues to be a lead partner of the Homes For Heroes charity, building tiny home communities for unhoused Veterans.
ABOUT THE ATLAS INSTITUTE FOR VETERANS AND FAMILIES
The Atlas Institute for Veterans and Families works with Veterans, Families, service providers and researchers to bridge the divide between research and practice so Veterans and their Families can get the best possible mental health care and supports. The Atlas Institute was originally established as the Centre of Excellence on PTSD and Related Mental Health Conditions, through the Minister of Veterans Affairs.
Quick facts:
- The Atlas Institute for Veterans and Families was established to provide easier access to information, research, tools and expertise on posttraumatic stress disorder (PTSD) and related mental health conditions.
- Since its inception, Atlas has contributed to the publication of numerous peer-reviewed articles and created various knowledge products, including fact sheets, written resources, videos and infographics. Atlas has led or is currently leading dozens of research projects and has partnered on many others.
- Atlas actively engages Veterans and their Families as key partners, co-investigators and co-authors of its research, including a process for their participation in reviewing research outcomes from a lived expertise perspective.
- It also collaborates and partners with Veterans and Families to understand which issues matter most to them, using that knowledge to work with them and with service providers and researchers to co-create resources and knowledge products that fit the unique culture and needs of the Veteran and Family communities.
OTTAWA, ON — March 13, 2024 — With the risk of suicide for Veterans 1.4 to 1.9 times higher than in the general population, and women Veterans almost two times more likely to die by suicide than women in the general population, Veterans and Families have long identified suicide prevention as a priority and emphasized the need for additional supports for mental health and well-being.
In recognition of this, along with the fact that early interventions and faster access to support can prevent the worsening of mental health conditions and contribute to improved overall well-being, the Atlas Institute for Veterans and Families has developed a suite of suicide prevention resources in collaboration with Veterans and Family members, and in partnership with the Centre for Suicide Prevention.
Fardous Hosseiny, President and CEO of the Atlas Institute, said, “Statistics confirm that the Veteran population is at a higher risk for mental health concerns than Canadian general population with reported rates among Veterans of 26% for depression, 24% for posttraumatic stress disorder (PTSD) and 21% for anxiety. These facts support upstream strategies focused on increasing protective factors,” he said, adding that tackling this issue must include equipping Veterans and Families equally with practical strategies and tools to understand and support their mental health.
The resources released on March 14 were co-created with an advisory committee made up of members of people with lived and living experience from the Veteran and Family community, including members of the Atlas Institute Lived Experience team. Laryssa Lamrock, National Strategic Advisor for Veteran Families at the Atlas Institute, who was involved in the resource development, explained that while Canadian Armed Forces and Royal Canadian Mounted Police Veterans are at higher risk of mental health concerns as a result of their service, their loved ones can also be significantly impacted when the Veteran is struggling with suicidal thoughts and behaviours. She noted that it is critical to acknowledge that Veteran Family members’ mental health is important to consider in its own right and that they may have their own challenges to be addressed.
“Our goal was to develop the new tools to support both Veterans and their Family members, so they can find answers based on the experiences of people like them for the questions they may have about mental health and suicide, be that immediate access to resources such as direct supports, tips and strategies for loved ones or for themselves outside of the needs of their loved ones. There is a continuum of experiences for both the Veteran and the Family member and these resources aim to acknowledge and support people’s needs at different points along that continuum.” Lamrock pointed to a recent Atlas-funded study that found there seem to be very few, if any, resources dedicated specifically to Family members in their own right, despite the fact they have their own mental health experiences and needs and may themselves be at risk for suicide.
Brian McKenna, a Veteran and National Strategic Advisor for Veterans at the Atlas Institute, agreed it is important for both Veterans and Family members to have suicide prevention resources that speak to their perspectives and unique needs. “These resources have been created for and by members of the Veteran community and include toolkits for both Veterans and Family members that incorporate their specific experiences. The Veteran toolkit looks at understanding suicide in Veterans, actions to take if someone sees warning signs in themselves or loved ones, and strategies to build resilience and help reduce risk among others. The toolkits include information and tips on self-care for Family members in their own right and for managing their own mental health and practical strategies to support their loved one.” McKenna added these are supported by a conversation guide that works through how to talk to someone who might be experiencing suicidal thoughts and behaviours, along with a help card that provides key pointers and information about direct supports for Veterans in crisis.
Mara Grunau, Executive Director of Centre for Suicide Prevention, said, “Veterans, Veteran Families and communities all have a role to play in building resilience and preventing Veteran suicide. If you’re worried about a Veteran, have an open, non-judgmental conversation. If they’re considering suicide, connect them to help.”
Hosseiny notes that for Veterans and Family members dealing with suicidal thoughts and behaviours in themselves and their loved ones, it can be overwhelming and difficult to know where to turn. “While there is work to be done, these resources are an important part of a much-needed multilayered approach to suicide prevention which can continue to grow. Our hope is to help Veterans and their Families know they are not alone and that this is a tool they can add to their toolkit to support both their own mental health and that of the person they’re caring for.”
Resources are now available to download and print at atlasveterans.ca/suicide-prevention.
For more information, please contact:
Rosemary Thompson
Artful Strategies
rosemary@artfulstrategies.ca
613-240-6739
Quick facts:
- The Atlas Institute for Veterans and Families was established to provide easier access to information, research, tools and expertise on PTSD and related mental health conditions.
- Since its inception, Atlas has contributed to the publication of 39 peer-reviewed articles and created more than 45 knowledge products, including fact sheets, written resources, videos and infographics. Atlas has led or is currently leading 14 research projects and has partnered on another 26 research projects.
- Atlas actively engages Veterans and their Families as key partners, co-investigators and co-authors of its research, including a process for their participation in reviewing research outcomes from a lived expertise perspective.
- It also collaborates and partners with Veterans and Families to understand which issues matter most to them, using that knowledge to work with them and with service providers and researchers to co-create resources and knowledge products that fit the unique culture and needs of the Veteran and Family communities.
OTTAWA, ON – September 22, 2023 – The Atlas Institute for Veterans and Families was honoured today by the visit of the First Lady of Ukraine, Olena Zelenska, leading a delegation to explore international leadership in supporting former military personnel and their Families in restoring their mental health and well-being post-conflict.
As part of the visit, a signing ceremony took place to formalize a memorandum of international Veteran and Family Mental Health partnership between the Ukrainian State Institution “Veterans Mental Health and Rehabilitation Center ‘Lisova Polyana’ of the Ministry of Health of Ukraine” and the research and knowledge mobilization institution, “the Atlas Institute for Veterans and Families” in Canada (hereafter — MOU). The MOU formalizes cooperation between the two organizations in Canada and Ukraine to explore possible collaborations for research, knowledge exchange and capacity-building in the sphere of mental health to best support people in Ukraine who have been impacted post-conflict.

“Together, we are looking to explore opportunities to collaborate that will allow Lisova Polyana to support Veteran and Family mental health in Ukraine, informed by the work Atlas is doing,” said Fardous Hosseiny, President and CEO of Atlas. “We believe that sharing experiences and knowledge related to Veteran and Family mental health systems of care can support the restoration and development of services across Ukraine’s health care system, and that this will position them for that long road to recovery.”
MaryAnn Notarianni, Deputy CEO and Executive Vice President, Knowledge Mobilization at Atlas, echoed this, noting that supporting the awareness, adaptation and joint development of information and psychoeducational mental health and well-being resources for Veterans and their Families as well as for the professionals who support them is a key aspect of the collaboration. She added, “As an organization that has cultivated a robust network of partnerships nationally and internationally to reduce silos and foster knowledge exchange around best practices for Veteran and Family mental health, this MOU aligns well with the mandate of Atlas. One of our initial steps will be to establish regular dialogue and the means to effectively communicate applicable research findings and best practices between Ukrainian and Canadian mental health professionals and researchers. With our internal subject matter experts (SMEs) and access to a network of other SMEs across Canada, Atlas is well-positioned to inform and advise on efforts to support the use of best-practice standards and protocols for quality mental health care delivery in Ukraine.”
“Through their research and expertise, and supported with funding from the Government of Canada, the Atlas Institute strengthens the care and support of Veterans,” said The Honourable Ginette Petitpas Taylor, Minister of Veterans Affairs and Associate Minister of National Defence. “Collaboration between the Atlas Institute and Ukraine’s Ministry of Health will help ensure that Veterans and Families in Canada and Ukraine benefit from shared knowledge and research in mental health.”
Hosseiny said that the realities of the current situation are a powerful reminder of the importance of focusing on the mental health of the population, while also ensuring tailored responses for groups like military members, Veterans and their Families who may be uniquely impacted. “As Atlas has championed awareness of Veteran and Family mental health needs in Canada, we are honoured to collaborate with our Ukrainian counterparts to support this effort in their country and model the way for engaging lived experience in that effort,” he added.
With the MOU now signed and the draft framework established, work will begin immediately to rapidly bring the collaboration together.
For more information, please contact:
Joy Pavelich
Executive Vice President, Communications and Public Affairs
Atlas Institute for Veterans and Families
joy.pavelich@theroyal.ca
1-403-934-1694
Quick facts:
- The Atlas Institute for Veterans and Families was established to provide easier access to information, research, tools and expertise on posttraumatic stress disorder and related mental health conditions.
- Since its inception, Atlas has contributed to the publication of 39 peer-reviewed articles and created more than 45 knowledge products, including fact sheets, written resources, videos and infographics. Atlas has led or is currently leading 14 research projects and has partnered on another 26 research projects.
- Atlas actively engages Veterans and their Families as key partners, co-investigators and co-authors of its research, including a process for their participation in reviewing research outcomes from a lived expertise perspective.
- It also collaborates and partners with Veterans and Families to understand which issues matter most to them, using that knowledge to work with them and with service providers and researchers to co-create resources and knowledge products that fit the unique culture and needs of the Veteran and Family communities.
OTTAWA, ON — June 29, 2023 — While peer support is widely practised in military and Veteran populations to help with recovery from service-related injuries as well as with adapting to post-service life, it can be challenging to find the peer support programs and services that are available to Veterans and their Families across Canada.
In response to a growing need to access this specialized support, the Atlas Institute for Veterans has launched an online repository and interactive map of Canadian peer support services for Veterans and their Families. The data used to create this resource was collected by the Canadian Institute for Public Safety Research and Treatment (CIPSRT) and shared with the Atlas Institute.
Until now, the extent of Veteran peer support activities has not been documented in Canada, nor have there been guidelines and standards in place to support these activities specific to this particular community, according to Fardous Hosseiny, President and CEO of the Atlas Institute. “Peer support has been shown to be effective in promoting well-being in a variety of settings,” Hosseiny said, adding that as part of their service, military personnel are trained to support each other and that mutual support ethic persists into life after service with peer support often occurring spontaneously among Veterans. “We know through our engagement with Veterans and their Families that peer support is an important component of their recovery journey. Our intention was to create a useful tool that ensures access to the Canadian peer support system.”
The interactive webpage, hosted by the Atlas Institute and guided by an advisory committee, provides both a map and list view that details where services are located and which services are offered anywhere in the country. The advisory committee is comprised of individuals across Canada who work or have worked in the field of peer support for Veterans and their Families at the national, provincial and local level. Their contributions were invaluable to the success of this project. Additionally, those searching for supports can filter by terms such as modality, language, cost, location and privacy/confidentiality, among others. Currently, there are 62 programs mapped from 40 unique organizations.
The Atlas Institute and CIPSRT are also collaborating on a network that will develop best practice guidelines to support the provision of peer support to Canadian Veterans, public safety personnel and their Families. This network consists of 41 members from coast to coast to coast. Currently there is not an official governing body or standardized guidelines that are specific to peer support for Canada’s Veteran community.
Hosseiny added that standardization in peer support delivery will help to ensure consistency in matters such as training, expectations on peer supporters and the ability to evaluate the quality of the service. “The advancement of best practice guidelines for providing peer support is central to this work, as well as ensuring a space for connecting peers and supporters, and promoting knowledge about the topic of peer support.”
To access the peer support map, visit atlasveterans.ca/peer-support-directory.
For more information, contact: media-atlas@theroyal.ca
OTTAWA, ON — June 13, 2023 — To fill the gap around educational resources on PTSI for young people in military and Veteran Families, the Atlas Institute for Veterans and Families has launched a new website, MindKit.ca, created for and by youth who have loved ones that have served in either the Canadian Armed Forces (CAF) or the RCMP.
MindKit.ca is filled with youth-friendly tools, strategies and downloadable resources as well as real-life stories from children of Veterans. The website features a webcomic, videos, audio clips, interactive tools and hands-on coping strategies to support youth whose lives have been impacted by their Family member’s mental health injury. All resources were co-created with a youth advisory group and subject matter experts.
Laryssa Lamrock, National Strategic Advisor for Veteran Families at the Atlas Institute, said MindKit.ca offers youth a central hub to learn about mental health and what it’s like to live with PTSI in the Family. “Not only is it about recognizing and validating the experiences through shared understanding, but the information on this site will also provide youth with different ways to handle challenges.”
Lamrock added that it is important to understand that the mental health of youth can be impacted by their loved ones’ mental health. “In homes where there is an OSI or PTSI, we know that children might take on caregiving roles for their parent or additional household responsibilities such as caring for younger siblings. These added responsibilities can have a cumulative impact on a young person’s well-being.”
Speaking to the impact on youth specifically, Fardous Hosseiny, President and CEO of the Atlas Institute, explained that early intervention and targeted resources can change the trajectory of a youth’s experience. “Research shows that children of parents living with mental health challenges are at risk for a number of emotional, behavioural and social problems and this could affect all areas of their lives. These impacts may manifest in various ways, including being confused, frightened or even angry with their parent or the situation. The children might blame themselves of feel ashamed of their Family situation.” Hosseiny added that being part of a community that understands their experience will go a long way towards reducing isolation and helping them realize they are not alone. In addition, it is important to reassure young people that supports are available and that their loved one’s injury is not their fault.
To explore the new website and resources, visit MindKit.ca.
For more information, contact: media-atlas@theroyal.ca
STAY CONNECTED
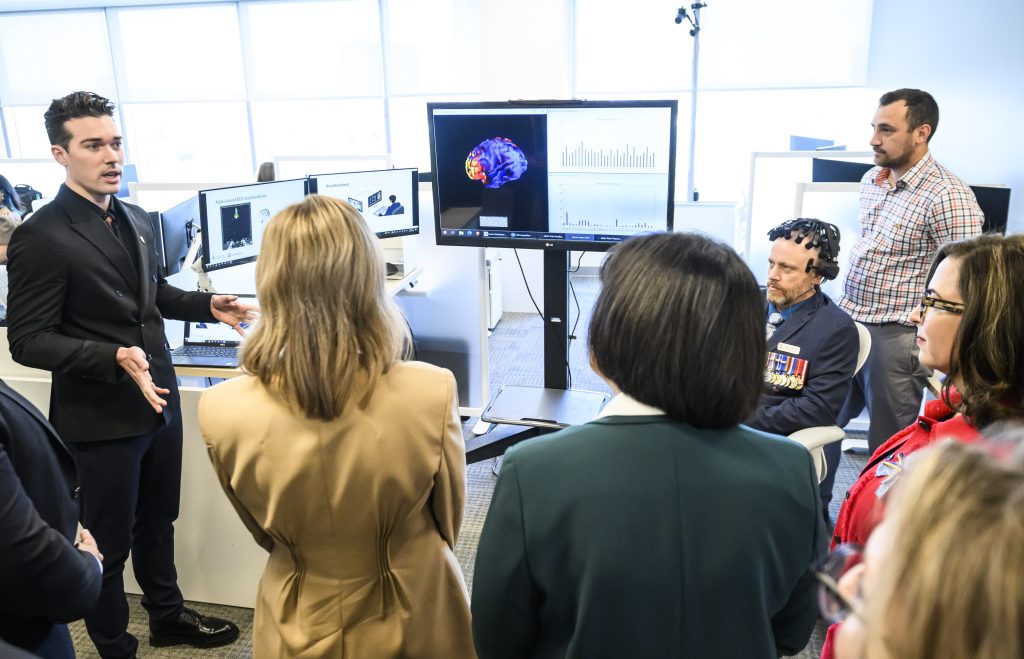
OTTAWA, ON – April 19, 2023 – Results of a recent international study show that neurofeedback, a non-invasive, non-pharmacological treatment, is indicating another promising option for the treatment of post-traumatic stress disorder (PTSD) with results showing it to be on par with gold standard treatments in terms of reduced symptoms and improved remission rates.
The trial collaboration between the Atlas Institute for Veterans and Families, Western University and the University of Geneva, shows how people can use neurofeedback to learn to non-invasively regulate brain areas that show altered activity (either too much activity or too little) in association with PTSD symptoms.
Dr. Andrew Nicholson of the Atlas Institute and scientist with the University of Ottawa Institute of Mental Health Research, along with Dr. Tomas Ros at the University of Geneva have been collaborators in this research program since its inception with Dr. Ruth Lanius at Western University. Speaking to her clinical experience in treating PTSD, Dr. Lanius said that neurofeedback has an intriguing ability to heal brain networks affected by trauma, and can be effective in helping individuals restore their sense-of-self and well-being in the aftermath of trauma.
Dr. Nicholson added that by regulating brain activity within these hypo/hyperactive areas, participants saw a decrease in associated PTSD symptoms. Dr. Nicholson stated, “The way neurofeedback works is that it provides the opportunity for individuals to train their brains in the same manner as one might work out muscles at the gym. Here, individuals learn to non-invasively regulate areas of the brain that can become dysregulated in the aftermath of trauma.” He added that he was especially encouraged by the fact that over 60 percent of participants not only experienced symptom reduction – they also no longer met diagnostic criteria for PTSD by the end of the trial. Dr. Nicholson also highlighted the tolerability of neurofeedback, saying, “Typically we would have seen a drop out rate much higher than this over the course of the trial, yet we actually didn’t have any patients leave the study. I think what this really speaks to is the tolerability and effectiveness of the treatment.”
This study is the latest milestone in a 10+ year research program on the use of neurofeedback for PTSD. Moving forward, Dr. Nicholson at the Atlas Institute will continue to collaborate with Drs. Lanius and Ros to expand this new frontier in PTSD treatments with the research being led out of the Atlas Institute.
President and CEO of the Atlas Institute, Fardous Hosseiny, said this is an exciting project for many reasons and he is happy to have the Atlas Institute catalyze this ground-breaking research. “It speaks to our ability and desire to explore new options for treatment of PTSD and other mental health problems,” Hosseiny said, adding that having many options is critical so that people can find what works best for them. “The range of treatments available to our community should be larger, so that Veterans and their Families can explore options to find what is going to give them the best quality of life possible based on their personal situations.”
The Atlas Institute will be hosting a webinar on June 1, 2023 that will bring together the perspectives of research, clinical application and, importantly, of those who live with the impact of PTSD: Veterans and their Family members.
For more information and to register, please visit: Neurofeedback: A promising new treatment for PTSD.
Learn more about neurofeedback therapy.

Canada’s Veterans often experience physical or psychological injuries as a result of their service — and sometimes both. Over the past several years, medical cannabis has emerged as a treatment area of significant interest to Veterans and their Families. In 2022, on the recommendations of their individual health care providers, more than 18,000 reimbursement claims were submitted involving cannabis for medical purposes through Veterans Affairs Canada.
A new report released by the Atlas Institute for Veterans and Families and the Mental Health Commission of Canada, titled Insights into Veteran and Veteran Family Experiences with Cannabis and Mental Health, summarizes conversations with the Veteran community from a dialogue series hosted during May and June of 2022. The sessions engaged Veterans, Family members, service providers and researchers in a discussion about their experiences and perspectives on cannabis use and mental health.
The report found strong interest among Veterans and Family members to explore cannabis as a treatment option for conditions such as post-traumatic stress disorder and to have more research and guidance on cannabis use and mental health.
“As one of the more than 18,000 Veterans approved by Veterans Affairs Canada to use medical cannabis, I was keen to participate in this collaborative project, as a community, our knowledge of cannabis is, in large part, based on our own experiences and the shared experiences of our peers. We are missing some of the key scientific and medical research necessary for us to make our own informed decisions about how cannabis may contribute to or jeopardize our other treatments,” said Major-General (Ret’d) Glynne Hines, chair of the Atlas Institute’s Veterans reference group, and project advisor and moderator for the dialogue series.
Additional insights:
- Health care professionals need more training and guidance on cannabis use for mental health.
- Cannabis use among Veterans continues to be highly stigmatized.
- Veterans need to know more about how cannabis works and interacts with other substances.
- The quality and independence of cannabis research matters; Veterans and Families want to be engaged in research.
- Knowledge, resources and actions must take diversity among the Veteran population into account.
Fardous Hosseiny, President and CEO of the Atlas Institute, said that while cannabis has potential as a tool to manage mental health conditions, more research needs to be conducted to explore the efficacy, impacts and best practices of cannabis as a treatment option for mental health conditions in Canada’s Veteran population. “What emerged from this dialogue series is that this is a significant topic of interest. There is a need for more research, resources, and guidance not only for Veterans and Veteran Family members but for the service providers who work with them, so that collectively they can be best-informed in their decision making around the use of medical cannabis.”
Mary Bartram, Policy Director at the Mental Health Commission of Canada, agreed that this project has shed light on the need for more nuanced research. “In order to honour the Veterans’ and Veteran Family members’ diverse experiences and help bridge the knowledge gaps between users and health care providers, we need to continue to advance evidence-based research hand in hand with the Veteran community.”
ABOUT THE ATLAS INSTITUTE FOR VETERANS AND FAMILIES
The Atlas Institute for Veterans and Families works with Veterans, Families, service providers and researchers to bridge the divide between research and practice so Veterans and their Families can get the best possible mental health care and supports. The Atlas Institute was originally established as the Centre of Excellence on PTSD and Related Mental Health Conditions, through the Minister of Veterans Affairs November 2015 mandate letter, with funding and budget announced in the March 2017 federal budget.
ABOUT THE MENTAL HEALTH COMMISSION OF CANADA
The Mental Health Commission of Canada (MHCC) leads the development and dissemination of innovative programs and tools to support the mental health and wellness of Canadians. Through its unique mandate from the Government of Canada, the MHCC supports federal, provincial, and territorial governments as well as organizations in the implementation of sound public policy. The MHCC has undertaken several initiatives to assess the impacts of cannabis use on mental health and inform future policy development. For more information on MHCC’s work in cannabis and mental health, please visit our website.
CONTACT
Media Relations
Mental Health Commission of Canada
613-683-3748
media@mentalhealthcommission.ca
Media Relations
Atlas Institute for Veterans and Families
media-atlas@theroyal.ca
The nature of the work of public safety personnel (PSP) means they are continuously exposed to potentially psychologically traumatic events. This can impact their mental health and well-being and increase their risk for developing post-traumatic stress injuries (PTSI) and post-traumatic stress disorder (PTSD).
In recognition of this, the Atlas Institute for Veterans and Families, in partnership with the Canadian Institute for Public Safety Research and Treatment (CIPSRT), has launched new educational resources and videos that share first-person experiences of PTSIs as well as helpful coping tips and strategies for PSPs, military members and their Families. These resources were created with the guidance of an advisory committee of current and former PSP and their Family members.
MaryAnn Notarianni, Deputy CEO and Executive Vice-President of Knowledge Mobilization at the Atlas Institute, says there are many reasons why PSP might find reaching out for help and support difficult. “The new videos and resources aim to help PSP and their Families recognize they are not alone, that support and resources are available and recovery is possible,” she said. “The objectives of developing these videos and resources are to reduce stigma, and then correspondingly to provide information that will support the well-being and help-seeking behaviours of PSP and their loved ones and caregivers. Acknowledging the issue is important, but having accessible supportive information is also crucial for the recovery journey to begin.”
Notarianni adds that these videos complement other resources the Atlas Institute has been producing for military and RCMP Veterans and their Families, acknowledging that many military members change one uniform for another and enter PSP roles when they transition to post-service life. “These videos add to the suite of resources the Atlas Institute has been developing to raise targeted awareness of PTSIs and the impact not only on individuals but Families as well.”
The videos feature seven first-person accounts from current and former PSP and their Family members, speaking to their personal experiences with PTSIs as a result of their work as first responders or other PSP or while supporting a loved one. There are also four educational videos providing information about PTSIs and how PSP and their Families can cope, with corresponding downloadable written resources, as well as a list of other helpful links, all featured at atlasveterans.ca/PSP.
Giselle Valaire, a community parole officer and member of the advisory committee for the project, says, “The perception is: ‘You’ve chosen this line of work, so you shouldn’t be affected by the trauma you have experienced.’ The culture is one of not showing weakness, especially as a woman.” She adds, “I suffered in silence for a long time because I did not want to be seen as weak by my co-workers or managers. I was worried others would judge me and lose faith in my ability to do my job. Mostly I was judging myself for being unable to cope with the environment I chose to enter.” Valaire says she feels it was important to use her experience to support others who might be dealing with their own struggles in silence.
Nicholas Carleton, Scientific Director at CIPSRT, echoes the need for PSP to have access to evidence-based resources that support the mental health and wellness of the community of individuals who work to keep Canadians safe. “We know that first responders and other PSP put their own lives on the line to keep others safe. By virtue of their work, PSP experience physical and psychological risks. We know that talking about mental health can reduce stigma, helping people to access evidence-based interventions earlier and supporting better health outcomes.” Highlighting the partnership between the Atlas Institute and CIPSRT, Carleton adds that organizations with complementary mandates can coordinate to help tackle complex challenges, allowing for further potential benefits for all who serve.
The project is funded by Medavie through the Medavie Foundation, as one of its community investment initiatives focused on helping first responders and Families impacted by post-traumatic stress injuries.
For more information, contact:
Over the past several months, there has been growing awareness about experiences of military sexual misconduct (MSM) and the resulting military sexual trauma (MST) among Canadian Armed Forces (CAF) members and Veterans. The Atlas Institute for Veterans and Families has responded to this important issue with the launch of a new collection of resources designed not only for individuals who are impacted by MST but also for health care providers who might be providing care and support to those affected.
MaryAnn Notarianni, Deputy CEO and Vice-President of Knowledge Mobilization at the Atlas Institute, said the Atlas Institute recognized early into its mandate that this was a key priority that would require significant attention, including the development of resources for those impacted. “We heard from the community about the numbers of people impacted, the devastating effects of MST and the need for dedicated resources,” she said. “This is a major public health concern, with one in four women and one in 25 men having experienced sexual assault at least once since joining the Canadian military.”
The resources released today have been developed in consultation with an advisory committee of Veterans with lived experience of MST and health care providers who work in the military/Veteran context, Notarianni added. “It is important to recognize the necessity of creating easily accessible resources for the individual, as well as of building critical awareness among health care providers. Through careful screening and training, more effective and sensitive physical and mental health care can be provided to people impacted by MST,” she said. “The resources were developed with the recognition that all providers, even those outside the military/Veteran community and the field of mental health, can support Veterans impacted by MST when they have the right tools available to them.”
“The first step in supporting and caring for someone is trying to understand how their MST impacts every facet of life. Not being understood is the worst human trauma in life. Every new research or resource we can develop and share strengthens every person’s healing path,”said MST survivor M.E. Sam Samplonius, CD.
“As a person with lived experience, my path has been brightened with more hope thanks to the work the Atlas Institute is doing for all of us and our loved ones.”
Major (Ret’d) Carly Arkell, one of two Veteran members of the working group on service provision who helped in the development of the resources, said the opportunity has been important for her own advocacy efforts in taking her experience and using it in support of others who might not yet have received the help and support they need. “I’m glad to have been part of developing these resources based on the real-life experiences of those of us who have experienced MST. Contributing in this way has been empowering — it has enabled us to share the unique challenges and experiences to add to the body of knowledge about the effect of MST, and to build meaningful support. With the development of these resources, I see the potential for change, which brings me hope, and we know hope can be a powerful thing.”
For individuals impacted by MST, there are two new resources providing tips, strategies and helpful information to support the healing journey — “Recovering from military sexual trauma: From coping to healing” and “Recovering from military sexual trauma: The role of peer support” — available both as downloadable, accessible PDFs as well as web resources.
The new resources for health care providers are designed to improve awareness of the unique military and Veteran-specific factors that can affect care for Veterans who have experienced MST. They include an introductory guide to MST, titled “Military sexual trauma: A guide for Canadian health care providers,” as well as an infographic and two brief videos that are focused on key practice tips for health care providers working with people impacted by MST.
The resources can be accessed on the Atlas Institute for Veteran and Families’ website at atlasveterans.ca/military-sexual-trauma.
For more information, contact: media-atlas@theroyal.ca