Neurofeedback therapy
A considerable number of people with posttraumatic stress disorder are treatment-resistant to currently available first-line interventions so the need to explore new and novel scientifically guided treatments is urgent.
A growing body of evidence shows that neurofeedback can help to treat posttraumatic stress disorder (PTSD) and other mental health issues. It trains people to self-regulate areas of the brain that may not be functioning well in the aftermath of trauma. This might include PTSD symptoms such as emotional reactivity or intensity, feeling on edge, vivid re-experiencing or flashbacks of the traumatic event, avoidance, disturbances in sleep and negative alterations in thoughts and moods.
A neurofeedback clinical trial was completed by researchers at the Atlas Institute, the University of Ottawa, Western University and the University of Geneva in 2023. At the end of the study, over 60% of participants no longer met diagnostic criteria for PTSD, with significant decreases in PTSD symptoms after receiving the neurofeedback treatment.
Additional research is currently underway to better understand and make the case for use of neurofeedback therapy in treating PTSD and related mental health conditions.
About neurofeedback
When people develop PTSD, certain parts of their brain can be over- or under-activated, triggering thoughts, emotions, moods and behaviours that can be unhelpful or distressing. These responses can happen very quickly and it is often hard for the person experiencing these feelings to know why they are happening. This contributes to making them hard to manage.
Neurofeedback is a non-invasive therapy, meaning that it doesn’t hurt or involve medication. It helps people learn how to self-control brain activity so that they can respond and think more clearly, balance their emotional responses and control triggered behaviours like avoidance, anxiety or panic.
Neurofeedback therapy can be used alone or along with other forms of treatment, such as psychotherapy, cognitive behavioural therapy (CBT) or medication.
There are two main types of neurofeedback therapy — one uses electroencephalography (EEG), and the other uses real-time functional magnetic resonance imaging (fMRI). EEG-based neurofeedback recalibrates brainwaves, while fMRI neurofeedback (a less commonly accessed therapy) recalibrates patterns of brain activity and connections between parts of the brain. Both forms of neurofeedback therapy allow clinicians to measure altered brain functioning resulting from trauma and provide feedback that helps individuals learn to self-regulate brain activity that can cause PTSD symptoms.
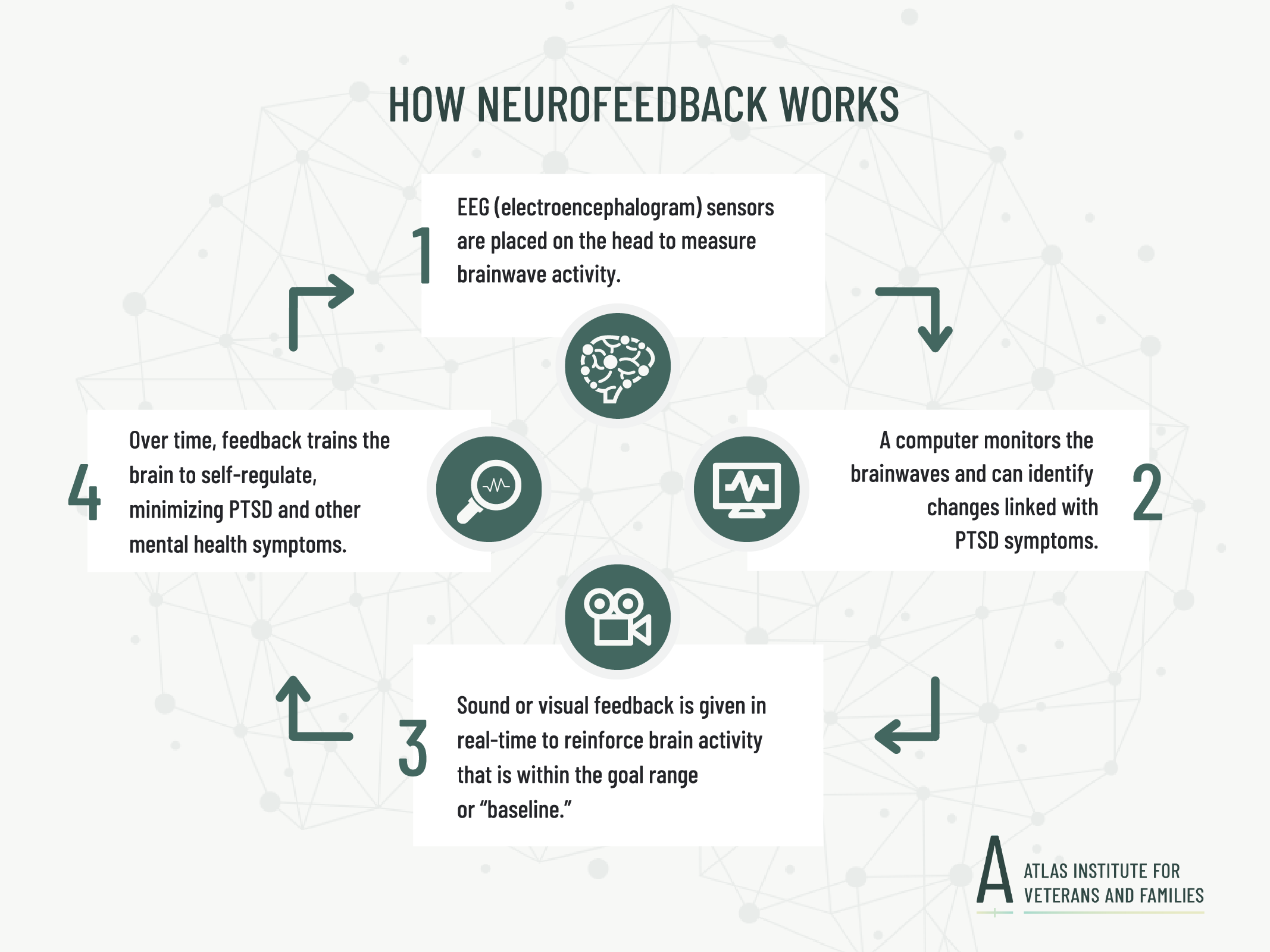
Neurofeedback therapy gives real-time feedback about brain activity from a computer-based program. For example, one form of neurofeedback uses an electroencephalography (EEG) machine to do this. Here, small metal discs (electrodes) are placed on the scalp, and the EEG machine records brainwaves (i.e., brain activity). This brain activity is then displayed in real-time through a feedback signal.
During neurofeedback training, the individual may be in a neutral resting state (i.e., similar to meditation practices) or given controlled trauma reminders as sounds or pictures. Brain activity is monitored as participants try to self-regulate.
Feedback about this brain activity is given immediately in the form of auditory or visual signals. This way, the participant becomes aware of the automatic responses the brain is having and that can cause symptoms of PTSD.
Over the course of neurofeedback therapy, individuals learn to train their brain to re-focus or regulate brainwaves in more balanced and helpful ways when triggers happen in the moment. That way, the triggers don’t result in unhelpful thoughts, emotions, moods and behaviours.
Neurofeedback doesn’t just treat responses to specific triggers – it can also help to improve functioning in day-to-day life.
At the start of the first neurofeedback session, a service provider will clearly explain the equipment and machinery being used, as well as the process.
Example of an EEG-based neurofeedback treatment:
- Clients are comfortably seated throughout the 20 to 60 minute session (although a variety of neurofeedback protocols exist, which can be tailored to benefit personalized needs).
- EEG sensors are placed on the client’s scalp using gel or a headband. The sensors only measure brain waves. They don’t have an electrical current so there won’t be a sensation of an electrical shock.
- Depending on needs and the particular treatment plan, clients view a video or animation (using a screen or headset) or listen to sounds or music that is streamed into the room or on headphones. This is usually related to the feedback signal, and changes over the treatment. Depending on the treatment needs, sometimes individuals will be shown words or pictures that are associated with their specific trauma experience (akin to exposure therapies for PTSD).
- The EEG sensors will measure brain activity as the client watches or listens.
- Visual or auditory feedback (i.e., a video or gentle beep) is given to the client when their brainwaves are within (or outside of) a goal range or “baseline.” For example, if the brain is reacting to a trigger and the EEG shows that the client is able to regulate it in the moment, the video may change slightly or they may hear a beeping sound to reward their brain for responding in a helpful way.
- This is repeated on a loop throughout individual sessions and for the course of treatment to train the brain to respond in more helpful ways when triggered.
As a non-invasive therapy, neurofeedback:
- Doesn’t hurt
- Does not require sedation or medications
- Does not always require exposure to trauma reminders.
After a neurofeedback session it is safe to return to regular daily routines. Some people may feel tired or mentally exhausted after the session.
Sometimes, individuals will have a pre-therapy session where they work with a trained service provider to “map their trauma.” In this process, individuals are asked to share the unique circumstances of the trauma they experienced, the particular symptoms they have and potential management strategies. The parts of the brain that show too much, or too little, activity that triggers PTSD symptoms may be identified, along with the particular cues that trigger those responses.
- Each session can last between 20 and 60 minutes.
- Sessions can be weekly or more frequent, based on needs.
- The duration of therapy varies for individual needs and is determined collaboratively by the service provider and the person receiving therapy.
- Importantly, more research is still needed to identify effective duration and dosing of neurofeedback treatments. This research is currently being conducted by the Atlas Institute.
Neurofeedback is safe, non-invasive and doesn’t have any known significant long-term side effects.
Accessing neurofeedback therapy
Neurofeedback/EEG biofeedback is approved by Veterans Affairs Canada (VAC) as an adjunct therapy for:
- PTSD
- Generalized anxiety disorder
- Major depressive disorder
If approved by VAC for coverage, neurofeedback can be reimbursed up to the appropriate fee as outlined in provincial fee guidelines of the health professional administering the treatment.
Neurofeedback therapy must be referred by a primary doctor or mental health professional (e.g. psychiatrist, psychologist or GP).
Learn more about accessing neurofeedback therapy through VAC.
A service provider who is covered through VAC/Medavie Blue will need to be certified by the Biofeedback Certification International Alliance, which offers a searchable database of clinicians here.
Service providers administering neurofeedback should have the appropriate training and be certified by the Biofeedback Certification International Alliance (BCIA). Only BCIA certified clinicians are covered under VAC/Medavie Blue Cross benefits.
Service providers should also have background and experience that is relevant to a client’s specific needs. For example, if the individual has a diagnosis of PTSD and/or another mental health concern, it will be important the neurofeedback service provider has knowledge and expertise in this area.
When considering working with a service provider, questions to ask include:
- What their educational background and credentials are.
- If they have experience working with Veterans and/or people with a diagnosis or symptoms like yours.
- What their process is like and what will happen during the sessions.
- How they will modify the treatment protocol if any side effects occur.
The Biofeedback Certification International Alliance offers a searchable database of clinicians here.
Neurofeedback/EEG Biofeedback therapy is covered under mental health services through VAC/Medavie Blue Cross for Veterans who qualify.
A recommendation from a primary doctor/mental health professional (e.g., psychiatrist, psychologist or GP) is required.
Learn more about how to qualify for neurofeedback coverage here.
Neurofeedback is covered by some private health insurance companies.
Research
To contribute to the growing body of evidence showing that neurofeedback is a promising treatment for PTSD and other mental health concerns, the Atlas Institute has initiated a program of research focused on exploring its efficacy.
Published Research
A tale of two targets
This preliminary research study begins to shed light on areas of the brain that can be targeted in neurofeedback therapy to decrease PTSD-related responses and reduce reliving and distress symptoms.
Though the amygdala (an area of the brain associated with emotional responses and fear/anxiety) has long been linked with PTSD symptoms, emerging research suggests that responses in this part of the brain don’t account for the full range of symptoms associated with PTSD. For example, the posterior cingulate cortex or PCC (an area of the brain associated with the self-reflection system that is related to dysregulated self-related emotional processing in PTSD) has been shown to be hyperactive during trauma cues in brain imaging in people with PTSD.
This research helps us to begin to understand and compare these two clinically relevant potential target regions in order to optimize future therapeutic protocols of neurofeedback to help people with PTSD.
A follow-up multi-session, sham-controlled, double-blind randomized control trial with a larger participant group is currently being led by the Atlas Institute’s Clinical Research team to help further test the findings in this research. You can find more about participating in this clinical trial by emailing atlasresearch@theroyal.ca.
Clinical trial showing EEG neurofeedback training can help with emotion regulation in people with PTSD
This international clinical trial collaboration between the Atlas Institute, the University of Ottawa, Western University and the University of Geneva shows neurofeedback to be on par with gold standard treatments for PTSD. Through a series of 20 neurofeedback sessions, participants were trained to regulate parts of the brain that show altered activity associated with PTSD symptoms.
- Over 60% of trial participants receiving active neurofeedback no longer met diagnostic criteria for PTSD, not just symptom reduction, by the end of the trial.
- No study participants left the trial, suggesting that neurofeedback therapy is highly tolerable and effective for patients.
- This was a double-blind randomized, sham-controlled trial of 40 participants with a primary diagnosis of non-dissociative PTSD.
Promising new intervention for treatment of PTSD
Fact Sheet
FAQs
Increased top-down control of emotions during symptom provocation working memory tasks following a RCT of alpha-down neurofeedback in PTSD
Homeostatic normalization of alpha brain rhythms within the default-mode network and reduced symptoms of PTSD following a randomized control trial of EEG neurofeedback
Study showing that people with PTSD experienced reduced reliving and distress symptoms as a result of fMRI-based neurofeedback targeting an area of the brain associated with emotion, thinking about oneself and memory
This international study collaboration between the Atlas Institute, the University of Ottawa and Western University shows that fMRI neurofeedback therapy can help to reduce reliving and distress symptoms associated with PTSD.
- This study aimed to investigate the effectiveness of functional MRI (fMRI)-based neurofeedback training in helping people with PTSD to regulate and strengthen an area of the brain associated with emotion, thinking about oneself and memory. This area of the brain is called the posterior cingulate cortex or PCC.
- The study showed that participants experienced reduced PTSD symptoms, such as reliving the experience and feeling distress as a result of neurofeedback training.
- fMRI scans showed neurofeedback can reset brain network connectivity that can be compromised for people with PTSD and that ultimately contribute to symptoms associated with disrupted memory, emotional difficulties, and altered thinking and thoughts about oneself or others.
- Results support PCC-targeted neurofeedback as a way to heal brain networks disruptions that contribute to PTSD symptoms.
Ongoing research
Other ongoing neurofeedback research studies being conducted by the Atlas Institute’s Clinical and Applied Research teams, and with partner organizations:
Multiple-session MRI-biofeedback study for PTSD at Lawson Health Research Institute, London, ON
What is biofeedback?
Biofeedback is a form of brain training to improve your health by learning to control signals from your own body.
Interested in participating?
You may be eligible to participate if you are between 18 to 65 years of age and have gone through a traumatic event, and experience any of the following:
- Vivid memories or nightmares of the trauma
- Unwanted or upsetting thoughts of the trauma
- Overwhelming feelings related to the trauma
Participation involves:
- 3 MRI scans
- Clinician-administered and self-report assessments
- Wearing a wristband device to measure sleep tracking
- Travel reimbursement
- Participation compensation for your time
Questions? Contact: jonathan.lieberman@sjhc.london.on.ca
Principal Investigator: Dr. Jean Théberge
If you are interested in participating in ongoing neurofeedback research trials, please contact us.
Note: Participating in research is not a treatment and benefits are unproven.
Find more resources
Browse the Knowledge Hub for more evidence-based information, fact sheets, reports and tips.